First Trimester Screening: The Complete Guide for Expectant Parents
First Trimester Screening (FTS) is your baby’s first “health check” between 12–13 weeks of pregnancy. It combines ultrasound markers and blood tests to assess the baby’s risk for certain genetic or chromosomal conditions early on — when decisions and planning actually matter.
Unlike diagnostic tests, FTS doesn’t confirm a disorder. Think of it as an early warning system that helps doctors understand if you need deeper testing.
Why Is First Trimester Screening Important?
This screening matters because:
- It detects early signs of chromosomal conditions like Down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Patau syndrome (Trisomy 13).
- It helps spot structural issues like early heart or abdominal wall defects.
- It gives insights into placental health, which can predict pregnancy complications later.
- It’s safe, non-invasive, and done early enough to make informed choices.
If there’s one time to stay on top of prenatal scans — it’s this.
When Is It Done?
FTS window falls between 12 weeks to 13 weeks
Do it too early — measurements aren’t accurate.
Do it too late — you miss the window for certain markers and early interventions.
What Does First Trimester Screening Include?
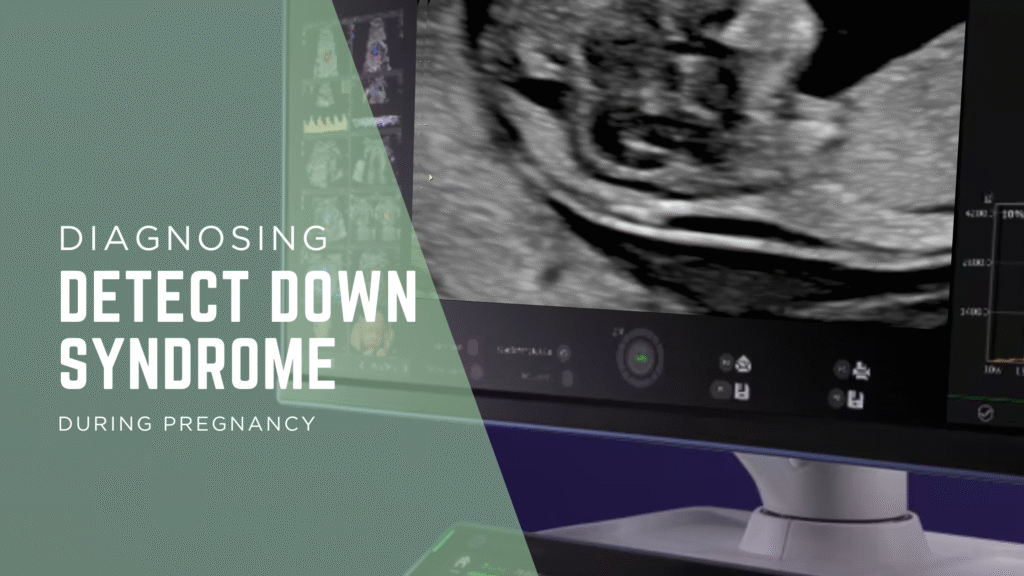
1. Nuchal Translucency (NT) Ultrasound
A specialized scan that measures the fluid at the back of the baby’s neck.
- Increased NT = higher risk of chromosomal abnormalities or heart defects.
- It also checks the baby’s anatomy, heartbeat, placental position, and gestational age.
2. Nasal Bone Assessment (NB)
Presence or absence of the nasal bone can be an indicator for Down syndrome risk.
3. Maternal Serum Markers
A blood test that measures two key proteins:
- Free β-hCG
- PAPP-A (Pregnancy Associated Plasma Protein-A)
The combination of NT + NB + serum markers gives a more accurate risk estimate.
What Conditions Can It Help Detect?
This screening helps identify the risk of:
- Down Syndrome (Trisomy 21)
- Edwards Syndrome (Trisomy 18)
- Patau Syndrome (Trisomy 13)
- Early indicators of congenital heart defects
- Early signs of placental dysfunction (linked to preeclampsia or growth restriction)
Again — it doesn’t confirm these conditions, but it signals if more testing is needed.
How the Risk Is Calculated
In first-trimester screening (FTS), multiple ultrasound and blood markers are combined statistically to provide an individualized “patient‑specific” risk ratio for conditions like Down syndrome, Edwards syndrome, and Patau syndrome. The final number (for example, 1:800 vs 1:50) reflects how likely the baby is to have a chromosomal condition compared with an unaffected pregnancy at the same gestation. Know more about how risks are calculated
The following markers are used to calculate the risk ration:
- Your age
- Baby’s NT measurement
- Nasal bone status
- Serum marker levels
- Baby’s gestational age
Once the risks are calculated, If :
- Low Risk → Routine care continues.
- High Risk → Follow-up tests like NIPT or diagnostic procedures (CVS/Amniocentesis) may be recommended.
Who Should Definitely Get First Trimester Screening?
Every pregnant woman can opt for it, but it’s especially important if:
- You are 35+ years old
- You’ve had previous pregnancies with genetic conditions
- You’ve had abnormal ultrasound findings
- There’s a family history of genetic disorders
- You want early reassurance and clarity
How to Prepare for the Test
Nothing fancy. Just:
- Drink some water before the ultrasound (helps visibility).
- No fasting needed.
- Carry your previous reports or early pregnancy scans.
You’re good.
What Happens If My Screening Result Is High-Risk?
Don’t spiral — high-risk doesn’t mean something is wrong. It simply means you need more precise testing like:
- NIPT (Non-Invasive Prenatal Testing) – safer, blood-based test
- CVS (Chorionic Villus Sampling) – an early diagnostic test
- Amniocentesis – confirmatory diagnostic test
Your fetal medicine specialist will guide you step-by-step.
Why Get Your First Trimester Screening at a Fetal Medicine Centre?
A specialized centre matters because:
- You get high-precision imaging
- Detailed anatomical evaluation (not just “NT-only”)
- Specialists trained in detecting subtle fetal anomalies
- Immediate counselling and next-step planning
- Integration with NIPT, CVS, and genetic counselling
Accuracy here isn’t just about the machine — it’s the expertise behind it.