Fetal Therapy at NESA Institute of Fetal Medicine
It can be overwhelming to learn that your baby may not survive or may be born with birth defects without medical intervention before birth. Fetal therapy exists to give families hope in exactly these moments. With today’s advanced imaging and minimally invasive procedures, doctors can diagnose and treat certain life-threatening conditions while the baby is still in the womb. Fetal therapy focuses on protecting the baby’s health, supporting the pregnancy, and giving parents the best possible chance at a positive outcome. At NESA, we approach every case with compassion, clarity, and the understanding that every family’s journey is unique.
The Evolution of Fetal Therapy
Fetal therapy has grown from a bold idea into one of the most remarkable achievements in modern medicine. In the early 1960s, Dr. A.W. Liley performed the first intrauterine blood transfusion — a breakthrough that proved treating the fetus directly was possible. Over the next few decades, pioneers like Dr. Michael Harrison expanded these possibilities with dedicated research, improved surgical tools, and advanced ultrasound imaging.
Today, fetal therapy is no longer experimental. It is a trusted, evidence-based option recommended worldwide when early intervention can save a baby’s life or prevent irreversible complications. Every milestone in this field has been driven by one goal: to give babies a fighting chance, even before birth.
Why Is Fetal Treatment Needed?
Fetal therapy is recommended only in conditions where intervention can genuinely improve the baby’s chances of survival or long-term health. These are situations where:
- The baby is at risk of death before birth
- A condition may cause severe, permanent organ damage
- Early treatment can prevent major disability
- Waiting until delivery is unsafe because the baby is too premature
The decision is never taken lightly. Fetal therapy is offered only when doctors see a realistic and meaningful benefit for the baby.
Conditions Where Fetal Therapy May Be Recommended
In some pregnancies, diagnostic results may reveal fetal conditions that can be treated before birth. Fetal intervention therapies such as intrauterine transfusions, fetal shunt placements, or laser procedures for twin-to-twin transfusion syndrome (TTTS) can significantly improve survival and long-term health outcomes. Fetal therapy may be advised for conditions such as:
- Severe fetal anemia (erythroblastosis fetalis)
- Complicated monochorionic twin pregnancies
– Twin-to-Twin Transfusion Syndrome (TTTS)
– TRAP sequence
– Selective growth restriction - Large fetal tumors causing hydrops
- Fetal heart failure due to structural or vascular issues
- Heterotopic pregnancy
- Cesarean scar pregnancy
- Select obstructive uropathies
- Cases requiring selective reduction for fetal survival
Your doctor will discuss whether fetal therapy is appropriate — and explain every option with transparency.
Fetal Therapy Options at NESA
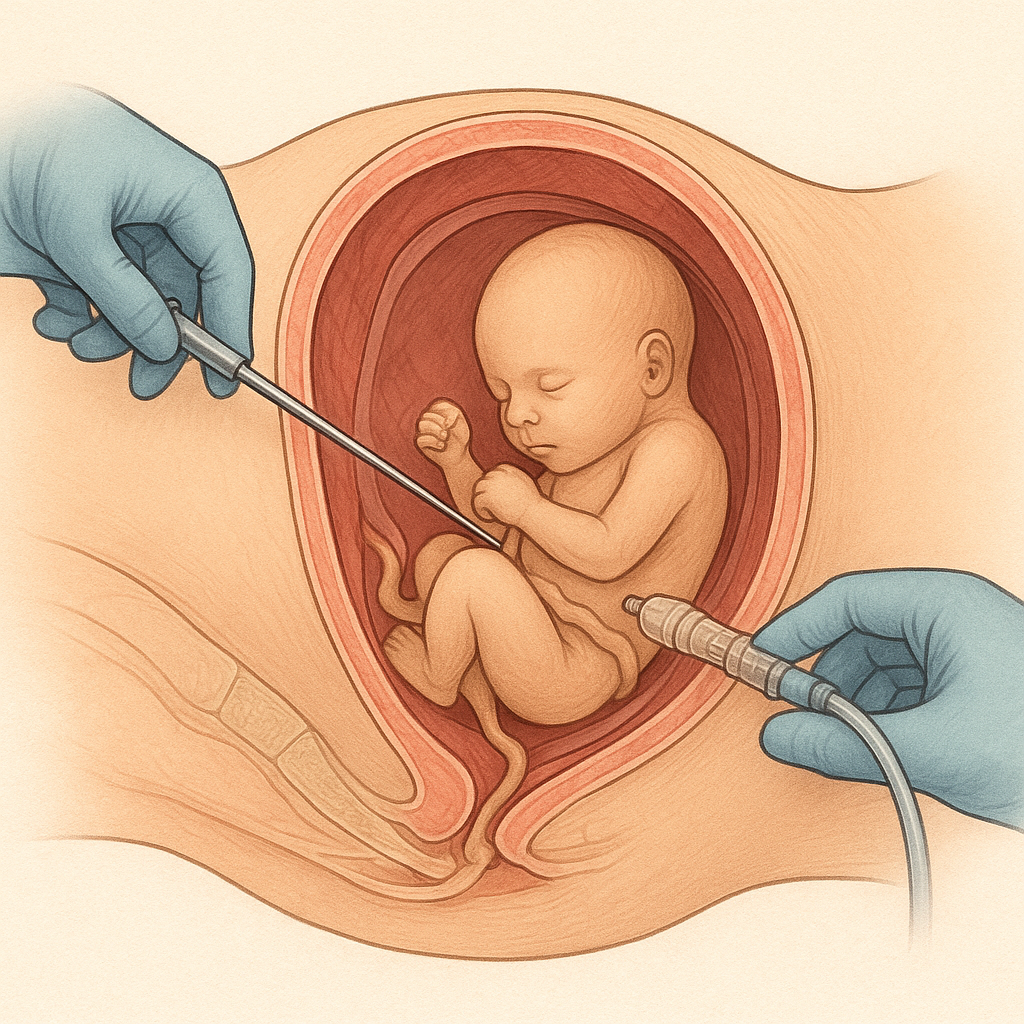
Each procedure below is performed under real-time ultrasound guidance, using the most minimally invasive approach possible.
1. Intrauterine Blood Transfusion (IUT)
A procedure where healthy donor blood is transfused directly to the baby through the umbilical cord to treat severe anemia. IUT has one of the highest success rates in fetal medicine. When performed at the right time, survival rates are typically 80–90% or higher. It is used conditions like Rhesus isoimmunization, Parvovirus B19 infection, other causes of significant fetal anemia
2. Radiofrequency Ablation (RFA)
A needle-based procedure that uses controlled heat energy to stop blood flow to an abnormal structure or a non-viable twin. RFA is a well-established therapy worldwide with healthy-twin survival rates around 70–80%, depending on the condition. commonly used for TRAP sequence, complicated monochorionic twin pregnancies and certain fetal tumors
3. Microwave Ablation (MWA)
A technique similar to RFA but uses microwave energy for quicker and more consistent tissue ablation, used for large or vascular fetal masses
4. Interstitial Laser Therapy
A thin laser fiber is inserted to seal abnormal blood vessels or treat affected tissues. Laser therapy has significantly improved survival and reduced complications in monochorionic twin pregnancies. It is used for :
- Select cases of Twin-to-Twin Transfusion Syndrome
- Selective reduction in complicated twin pregnancies
- Vascular malformations or tumors
5. Minimally Invasive Ultrasound-Guided Procedures
A range of needle-based procedures performed without open surgery. These procedures often stabilise the baby’s condition and prevent further damage, giving time for growth or safe delivery. Used to treat conditions like Polyhydramnios, Pleural effusions, Select urinary obstructions
This Includes procedures like:
- Amnioreduction
- Thoracocentesis
- Fluid drainage procedures
- Shunt placements (in select conditions)
6. Management of Heterotopic Pregnancy
A targeted treatment to safely address the ectopic pregnancy while preserving the intrauterine pregnancy. Early treatment can help preserve the normal pregnancy in 70–80% of cases. It is used t treat Coexisting ectopic and normal pregnancies (more common with IVF).
7. Management of Cesarean Scar Pregnancy (CSP)
A careful, minimally invasive approach to treat a pregnancy implanted in the cesarean scar. It is used for Early-detected CSP, and Cases where medical treatment alone is not enough