Fetal Well-being Scan Red Flags: What Parents Need to Know in Kolkata
Pregnancy in its final weeks is an exciting yet anxious time. While most ultrasounds reassure couples that all is well, the 36–40 week fetal well-being scan can occasionally uncover “red flags” that require attention. Knowing what these warning signs mean—and the proactive steps to take—can make a world of difference for a safe delivery.
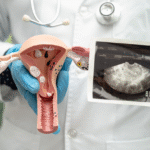
What Is the Fetal Well-being Scan?
The Fetal Well-being Scan is a detailed ultrasound exam usually offered between the 36th and 40th week of pregnancy. Unlike earlier scans, this one zeroes in on the baby’s overall health, growth, and readiness for birth. The intent is simple: to answer any last-minute questions about your baby’s status and ensure there are no hidden issues before delivery.
Why This Scan Is Important
Late in pregnancy, fetal risks and complications can sometimes surface unexpectedly. The well-being scan offers important insights:
- Checks on Growth and Weight: Ensures the baby is growing as expected, reducing surprises during delivery.
- Monitors Amniotic Fluid: Assesses the cushioning and protection for your baby; too little or too much fluid may signal complications.
- Reviews Placental Function: Determines if your baby is receiving enough nutrients and oxygen.
- Baby’s Position & Movement: Confirms the safest route for delivery, detecting breech or transverse positions.
- Vital Signs and Doppler Studies: Evaluates heart rate, blood flow, and overall fetal status using advanced imaging.
What Are “Red Flags” in the Fetal Well-being Scan?
What Do They Mean for Parents?
Your doctor interprets scan results through several critical checkpoints. Some findings may require further Care. Common Red Flags Detected in a Well-being Scan include:
Fetal Growth Restriction (FGR) or Macrosomia (Large Baby)
- Fetal Growth Restriction (FGR) is a condition where the baby is smaller than expected for their gestational age, often due to problems with the placenta that limit the supply of oxygen and nutrients. Babies with FGR are at higher risk for complications during labour and after birth, such as low blood sugar, infection, and developmental delays.
- Macrosomia refers to a baby that is much larger than average—typically over 4 kg (8 lbs 13 oz) at birth. Large babies may face issues like difficult deliveries, birth injuries, or require a cesarean section for safety. Detecting these conditions early helps the doctor plan for a safer birth and specialized care if needed.
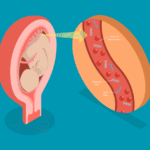
Abnormal Amniotic Fluid Levels
Amniotic fluid surrounds and protects the growing baby. Low levels (oligohydramnios) can restrict movement and affect lung development, while high levels (polyhydramnios) can signal problems such as gestational diabetes or birth defects and may increase the risk of premature labour. Detecting fluid imbalances allows doctors to monitor the pregnancy closely, recommend interventions, and reduce risks during delivery.
Placental Aging, Detachment, or Placenta Previa
- The placenta is responsible for nourishing and providing oxygen to your baby. As pregnancy advances, the placenta may begin to age and function less efficiently (“placental insufficiency”), affecting the supply of nutrients.
- Placental detachment (abruption) is when the placenta separates from the uterine wall too early, which can be dangerous for both mother and baby, potentially causing heavy bleeding and distress.
- Placenta previa describes a placenta that is covering or very close to the cervix, blocking the baby’s passage and making a normal vaginal delivery risky or impossible. Early detection through scanning is key to planning the safest method of delivery.
Abnormal Umbilical Cord Blood Flow or Cord Entanglement
- Doppler studies during a well-being scan evaluate blood flow in the umbilical cord. Abnormal flow may mean the baby is not getting enough oxygen or nutrients, a condition that can impact growth or cause distress.
- Cord entanglement or a “nuchal cord” (cord around the baby’s neck or body) is common and rarely dangerous, but in some cases can affect blood flow or complicate the birth process. These findings may prompt additional monitoring or adjustments in birth plans.
Breech or Transverse Position
Ideally, babies settle in a “head-down” position ready for birth by the end of pregnancy. Breech position means the baby’s buttocks or feet are facing down, while transverse means lying sideways. Both positions can complicate vaginal delivery and may require planning a cesarean section or attempting special manoeuvres to turn the baby before labour begins.
Fetal Distress Signs
Fetal distress refers to warning signals that the baby may not be coping well inside the womb, often indicated by abnormal heart rate patterns, reduced movements, or changes in Doppler studies. This can be due to lack of oxygen or other underlying problems. Timely identification allows immediate interventions, such as enhanced monitoring, hospitalization, or early delivery to protect the baby.
What Happens Next?—Practical Steps When a Red Flag Appears
- Enhanced Monitoring: Expect more frequent checkups to track your baby’s status.
- Repeat Scans or Further Tests: Non-Stress Tests (NSTs), biophysical profiles, or repeat ultrasounds may be scheduled.
- Specialist Referral: If needed, NESA’s maternal-fetal medicine team will involve senior experts or related specialists.
- Planning the Birth: Your doctor may recommend induction, a scheduled cesarean, or close monitoring during labour.
- Informed Support: Our team will explain every finding to you and your family so you feel supported and empowered.
Why Early Action Matters
Explain that quick recognition and clear planning result in healthier outcomes for mother and baby—and offer reassurance that most red flags can be managed effectively with expert care.
Conclusion
Spotting a red flag during the fetal well-being scan doesn’t mean there’s reason to panic—it means you and your care team are staying one step ahead. With timely interventions and expert support from NESA Institute of Fetal Medicine, you can look forward to a safer and more confident birth experience.
Worried about your scan results or need a second opinion?
Contact NESA Institute of Fetal Medicine at +91 92306 49133. NESA’s Team of Fetal Medicine Experts are here to help you every step of the way.